SPONSOR CONTENT
These Innovative Minds Are Giving Us Real Answers to Cancer
Since the 1960s, the five-year survival rate for many blood cancer patients has doubled, tripled, even quadrupled.
In 1964, the chance of surviving acute lymphocytic leukemia (ALL), the most common childhood leukemia, was 3%. Today it’s 90%.
Thanks to brilliant science over the last 60 years, hundreds of thousands of blood cancer patients today live normal lives. Many manage their condition with just a daily pill, instead of suffering the misery of more toxic chemotherapy treatments or radiation, as in years past.
Gleevec® was one of the first of these daily pills. Developed in the late 1990s with help from The Leukemia & Lymphoma Society (LLS), Gleevec made the cover of Time and holds the record for the drug with the fastest approval by the FDA.
“Now instead of blood transfusions, staggering fatigue, persistent nausea and infections, I can walk marathons,” says Virginia Garner, one of the first people in the world to take Gleevec as standard treatment.
Converting a fatal cancer into a manageable chronic disorder is a miracle. But incredibly, that was accomplished 14 years ago. What have scientists done for us lately?
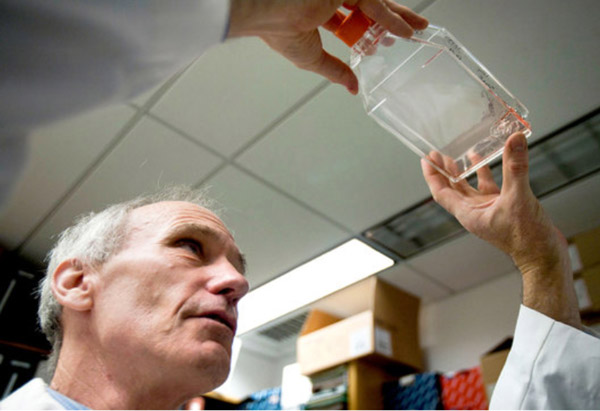
Teaching human cells to be cancer killers. The experimental work with advanced leukemia patients being done by a research team at the University of Pennsylvania and Children’s Hospital of Philadelphia has a lot of people crossing their fingers.
Led by Penn Medicine’s Carl June, M.D., the team is developing new approaches that selectively boost a patient’s immune system.
Dr. June’s team harvests T cells that normally fight viruses, programs them to attack cancer, then puts these re-engineered cells back into the bloodstream—and into battle.
The results are shifting expectations about how to treat patients who no longer respond to standard therapies. Two of the first three adult patients to receive the therapy remain in complete remission more than two-and-a-half years after their treatment, and the first pediatric patient has been in remission for a year. Dr. June and his team, as well as other research teams around the country, are accomplishing what researchers have hoped to do for decades: Train our immune system to kill cancer cells.
Getting through the system faster. Ibrutinib (pronounced “ee-brew-tin-ib”) is a new drug that targets an enzyme that promotes cancer cell growth. Available as a pill, it is proving to be effective in treating patients with aggressive chronic lymphocytic leukemia (CLL) and forms of non-Hodgkin lymphoma (NHL).
Importantly, Ibrutinib eliminates the need for toxic and less effective chemotherapy agents, which allows for continuous dosing.
John C. Byrd, M.D., of The Ohio State University, is a world-renowned CLL expert who leads an LLS-funded research team that has been instrumental in developing new therapies including ibrutinib. Ibrutinib has just received a “Breakthrough Therapy” designation, which allows expedited FDA review and development of a drug for serious or life-threatening conditions.
This status allows the drug to move faster through the approval process, ultimately getting it to the patients who need it faster and saving lives. This is quite an accomplishment when you consider that it usually takes 7 to 10 years to get a cancer drug from the lab to the clinic.
A new weapon against the most common adult lymphoma. A new drug has been identified that inhibits the protein BCL6, which promotes the growth of cancer cells in diffuse large B-cell lymphoma (DLBCL), the most common form of lymphoma in adults.
About to enter its first human clinical trial, the drug is called RI-BPI. It was identified by Ari Melnick, M.D., of Weill-Cornell Medical College, who collaborated with other researchers in New York as well as another LLS-funded research team in Chicago.
This is an astounding development that gives adults diagnosed with lymphoma new hope for a better life, and may also help patients with acute lymphocytic leukemia (ALL) and some forms of breast cancer.
A stunning advance for a high risk disease. Finally, the scientists of Celator, a small biotech company based in Princeton, New Jersey, and Vancouver, B.C., have developed CPX-351 for patients with secondary acute myeloid leukemia (AML), a high-risk form of the blood cancer.
Prognosis for secondary AML is usually grim. And unfortunately, because there is such a small patient population, there have been few advances for AML patients in the past 30 years. So this is a very significant discovery.
CPX-351 is a special combination of two standard chemotherapy drugs that delivers higher efficacy and less toxicity. In clinical trials that tested CPX-351 against the standard delivery of the same two drugs, CPX-351 almost doubled the number of patients who achieved complete remission, and nearly tripled the number of people surviving one year after treatment.
The good news is, we could go on and on. The amount of blood cancer research – and stunning breakthroughs—is making a real difference for many patients and their families, for today and into the future.
Each of the doctors and researchers mentioned here has been supported over the years by The Leukemia & Lymphoma Society—which has been supported for over 60 years by generous financial gifts from farsighted individuals, who view their donations as the most rewarding investment they can make: an investment in saving lives.
For more information on how you can make a difference, go to www.lls.org.



